How to Avoid Hangovers, According to Doctors and Dietitians
Read the article to learn lots of useful tips for avoiding hangovers.


Read the article to learn lots of useful tips for avoiding hangovers.

There are many effective treatment options for ED. This condition can be successfully reversed in more than 19 out of 20 men. Which treatment options work best may depend on ED’s underlying causes, as well as your own needs and preferences.
Erectile dysfunction is often caused by changes to your hormones, vascular system (heart and blood vessels), nervous system, or mental health. If you are experiencing ED, your doctor may want to perform a general health check-up to see whether it might be caused by another factor, such as an underlying health condition or medication.
When ED occurs, it could be a sign that something else is going on with your health. For example, one common cause of ED is diabetes. Men with diabetes are three times more likely to develop erectile dysfunction, compared to men without diabetes. If you experience ED along with other diabetes symptoms, such as frequent urination, extreme thirst or hunger, or unexpected weight loss, tell your doctor. Diabetes can be managed with proper diet, exercise, or medication.
Erectile dysfunction may also be caused by:
ED can also develop after certain cancer treatments. Surgery for prostate cancer or bladder cancer can cause the condition. Additionally, other prostate cancer treatments such as radiation therapy to the pelvis and androgen suppression therapy may lead to ED.
Treating an underlying disorder may help improve ED symptoms. It’s important to talk to your doctor if you start experiencing this condition.

Some mental disorders or emotional factors can cause erectile dysfunction or make it worse. ED can be a symptom of both anxiety and depression. Feelings of guilt, fear, or low self-esteem surrounding your sexual performance can also cause ED. Finally, men are more likely to experience ED when they are stressed or tired.
Talking to a counselor, therapist, or another mental health professional can help with all of these issues. These health providers can teach you techniques to better manage stress, reduce anxiety or depression symptoms, or reframe your attitudes surrounding sex. For some men, counseling is the most effective ED treatment.
Medications that can lead to ED include:
If you develop ED after trying a new drug or switching medication doses, talk to your doctor. You may be able to try an alternative treatment plan that won’t cause this side effect. However, it’s important to not stop taking a drug without first talking to your doctor, as some medications shouldn’t be stopped abruptly.
Your daily habits and choices can sometimes create or exacerbate problems with ED. Making some or all of the following changes may help:

There are several drug options that can help treat ED. They include:
These medications enhance natural processes in the body that cause erections. A chemical called nitric oxide is partially responsible for erections. It relaxes muscles within the penis and widens blood vessels, boosting blood flow.
Oral (taken by mouth) ED medications strengthen nitric oxide’s natural effects. They can make it easier for you to experience erection when you are sexually aroused.
Sildenafil, tadalafil, vardenafil, and avanafil are generally safe to take for most men. However, men with certain conditions should avoid these medications. These drugs may not be safe if you:
Oral ED medications often don’t cause any major side effects. However, some men may experience certain health changes while using these drugs, including:
If you are interested in using oral ED medications, ask your doctor about possible positive and negative effects. Your doctor can also help you understand whether you can take these medications safely based on your personal health history.
Each of these ED medications may lead to slightly different side effects and last for different lengths of time. For example, sildenafil and vardenafil typically last four to five hours, avanafil’s effects continue for up to six hours, and tadalafil can last for 36 hours.
Doctors often first recommend sildenafil for erectile dysfunction because this drug was developed first and it has been studied the longest. However, you may find that you prefer a different medication based on its effects or financial costs. You may need to try more than one medication or adjust your medication dose before you find something that works well for you.
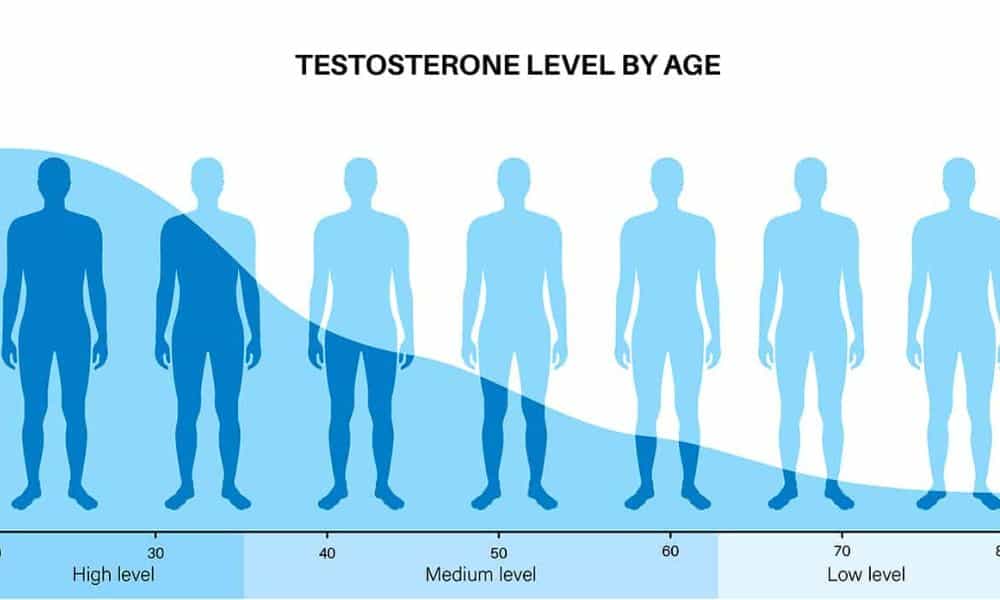
Testosterone is a sex hormone that plays a role in sexual development and fertility, and sexual function, including erections. The amount of testosterone in the body decreases with age, and can also drop due to changes in the brain, problems with the thyroid (a gland that makes hormones), testicular damage, or obesity. Low levels of testosterone are sometimes responsible for ED.
Low testosterone levels could also cause symptoms like:
If your ED is caused by low testosterone levels, you may be able to try testosterone replacement therapy (TRT). This involves taking medications that contain laboratory-made testosterone in order to elevate hormone levels in the body. This medication may come in the form of a pill, patch, implant, patch, or injection.
TRT may come with some side effects, such as:
TRT may interact with certain medications, and only works if ED is caused by certain factors, so talk to your doctor before trying this therapy.
A couple of other medication options besides pills may also help with ED. One option is Caverject (alprostadil), a drug that is injected into the penis. This medication encourages blood to flow into the penis, making it become erect. The injection usually leads to an erection within five to 20 minutes, and the erection typically lasts between 30 and 60 minutes.
Alprostadil can also be used as a urethral suppository — a small pellet placed into the opening of the penis with an applicator. This form of alprostadil generally causes an erection within 10 minutes and its effects also last 30 to 60 minutes.
Alprostadil can lead to side effects like bleeding or bruising at the injection site, pain or burning in the penis or surrounding tissues, headache, back pain, or vision changes. Before using alprostadil injections or suppositories, tell your doctor if you are taking blood-thinning medications or using drugs to treat high blood pressure, allergies, or a cold.
Another possible ED treatment is a vacuum device or penis pump. To use this device, you place a plastic tube around your penis and use a pump to draw air out, which causes more blood to flow into the area. After achieving an erection, you place a ring around the base of your penis to keep your blood, and your erection, in place.
Vacuum devices may cause bruising, or make your penis feel cold or numb. However, most men experience orgasm normally after using this device.
The above treatment options will work for most men. However, in some cases a man may choose to try surgical ED treatments.
In one type of surgery, a doctor can implant a device into the penis. This may be an inflatable device connected to a pump in the scrotum, or a flexible rod that allows a man to move his penis into the desired position.
Some cases of ED are caused by a blocked blood vessel that prevents blood from reaching the penis. In this case, the blood vessel may be able to be fixed with surgery.
Companies make many “natural” medicines or supplements that they say can treat ED. Some of these products may help improve sexual function, while many come with some risks.
Some studies have identified natural herbs or supplements that could possibly help ED and appear to be safe when taken at recommended doses. These include:
Although these supplements are often labeled as “natural” and are available without a prescription, you should still tell your doctor if you choose to use them. Some of these herbs, like ginseng, are only known to be safe when men use them for the short term. Other supplements, like L-arginine, shouldn’t be combined with other ED medications like sildenafil.
Not all supplements are safe. The U.S. Food and Drug Administration (FDA) has identified hundreds of supplements that contain drug ingredients not listed on the label. These supplements can sometimes cause serious health problems.
Some online retailers also claim to sell “herbal” versions of common prescription ED medications. These supplements are often not legitimate and can contain harmful substances.
In order to minimize risks, only take medications that are recommended by your doctor. It’s also a good idea to avoid products that claim to work very fast, are sold as single doses or were advertised to you through unsolicited emails.
There are many places online where you can buy ED treatments — both supplements and prescription medications. Unfortunately, many retailers run scams or sell counterfeit treatments.
Keep yourself safe by only buying treatments from reputable pharmacies, whether online or brick-and-mortar. Some good rules to follow include:
The therapy that is most effective for someone else may not be the one that is best for you. The ideal ED treatment plan depends on factors like what is causing your condition, how severe your ED is, and whether you have other health conditions that contribute to your ED.
Your doctor can help you understand which treatment might be best for you and the benefits and drawbacks of each option. They can also prescribe any medications that you may need. It can be pretty tough to bring up this topic with your doctor but initiating that conversation can be the key to curing your ED and improving your well-being. If you or your loved one is experiencing ED and you would like to discuss it with a doctor, please make an appointment with Dr. Connor.

In an article in Giddy, Dr. Connor explains that although menopause is a natural part of life, the symptoms often cause women to seek treatment. Read this entire article to find out how CBD oil works in the body and if it can be beneficial toward eleviating menopausal symptoms. If you are being impacted by menopausal symptoms and would like to discuss this further with Dr. Connor, please make an appointment.



However, the sun can also harm your skin if you’re not careful. Sunlight can damage skin cells, leading to signs of premature aging such as wrinkles, an uneven skin color, and a leathery appearance. Too much sun can also lead to eye diseases. Importantly, sun exposure is also the main cause of skin cancer. Therefore, it’s important to keep yourself safe when you’re outdoors.
Skin cancer develops when skin cells become damaged and begin growing too quickly. If left untreated, cancer cells can move from the skin to other parts of the body.
About one in five people in the U.S. will develop skin cancer at some point in their life. It is the most common type of cancer for people living in the U.S.
There are a couple of different types of skin cancer. The two most common types are basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). The more sun you get throughout the course of your life, the higher your risk of developing BCC and SCC. Another type of skin cancer, melanoma, is rare but is more aggressive and harder to treat. The more sunburns you received in your teenage years, the higher your chances of being diagnosed with melanoma.
Cancer develops when a cell’s genes — sets of instructions that tell the cell what to do — become changed or mutated. This causes the cell to begin dividing out of control, forming many new cells that make a tumor.Skin cancer is primarily caused by sunlight, which contains ultraviolet (UV) rays that harm skin cells. There are two main types of UV rays that play a role in skin cancer. UV-A rays can infiltrate into deeper layers of the skin, where they form free radicals (tiny molecules that can damage many parts of the cell, including the cell’s genes). UV-B rays mainly stay in the outermost layer of skin and cause changes in DNA, the material that makes up genes.
Certain risk factors can increase your chances of developing skin cancer. These include:
People without these risk factors can still develop skin cancer. However, skin cancer is more common in people with these features.

Studies have mostly found that using sunscreen can decrease skin cancer rates.
In particular, one large clinical trial conducted in Australia instructed some of the study participants to apply sunscreen every day, while the rest of the participants were free to decide when they put on sunscreen. After 4.5 years, the people who used daily sunscreen were 40% less likely to have SCC, the second most common skin cancer type.
After 15 years, the researchers followed up with the study participants and found that they were also less likely to experience melanoma, the most aggressive form of skin cancer. Other, smaller studies have also found that using sunscreen can reduce rates of SCC and of actinic keratosis, a condition that can develop into skin cancer.
Interestingly, this clinical trial did not find that sunscreen helped protect against BCC — people who used daily sunscreen and people who did not developed this skin cancer at similar rates. Experts speculate that this may be because BCCs take a very long time to develop. Longer studies are needed in order to determine whether sunscreen can prevent BCC.
Research has also found that sunscreen can help prevent wrinkles, uneven skin coloration, and spider veins (small blood vessels that appear close to the skin’s surface, leading to reddish lines on the skin).
Overall, experts such as the Centers for Disease Control and Prevention (CDC) and the American Academy of Dermatologists (AAD) recommend using sunscreen when spending time in the sun.
Everyone should put on sunscreen before going outside. Even people without skin cancer risk factors can develop the condition, so sunscreen can help all people, regardless of their age, race, and other factors.
However, experts recommend not applying sunscreen to infants younger than six months. These children may be more likely to experience a skin rash or other side effects. Instead, keep your newborn in the shade, dress them in clothing and hats that cover their skin, and make sure they stay well-hydrated with formula or milk.
Sunscreen should be worn every day for the best protection. UV rays can pass through clouds, so you can still experience sun damage even if it’s not a sunny day. Additionally, you are still exposed to UV light during the daytime even when it’s cold outside.
Sunscreens are rated based on their sun protection factor (SPF). The SPF measures how much UV light the sunscreen protects against. The higher the SPF, the more you are protected.
The CDC recommends using at least SPF 15 sunscreen, while AAD recommends SPF 30. Some experts believe that higher SPF ratings may be more helpful, because people often don’t apply enough sunscreen. For example, if you are using SPF 30 sunscreen and only apply half the recommended amount, you may only be getting the equivalent of SPF 15 protection.
The CDC and AAD also suggest making sure your sunscreen protects against both UV-A and UV-B rays. It also helps to use sunscreen that is water resistant if you’re planning on swimming or think you may end up sweating a lot.
Make sure you’re putting on enough sunscreen. Experts recommend using an ounce of sunscreen over your entire body. This is enough sunscreen to fill one shot glass. Make sure to cover all of your skin, including your ears, the tops of your feet, and — if you have short hair — your scalp. Additionally, use lip balm with an SPF of at least 30 to protect the skin of your lips.
Sunscreen works best when it is applied at least 15 minutes before you go outside. Reapply every couple of hours, or after you swim, towel off, or sweat.
Sunscreen can occasionally lead to reactions such as stinging, burning, or a rash. They may also clog the pores. In some cases, people may be allergic to certain sunscreen ingredients, but this is rare.
Some people worry that certain sunscreen ingredients may not be safe if they are absorbed into the bloodstream. In particular, there has been concern about two common ingredients — oxybenzone (BP-3) and octinoxate (OMC). So far, studies have not found any strong links between these ingredients and health problems, although researchers are continuing to look into this area.
It is important to note that sunscreens containing BP-3 or OMC have been banned in Hawaii and in Key West, Florida. This is because these ingredients may harm coral reefs and negatively impact plants and animals that live in the water. Avoiding sunscreens with these ingredients may be better for the environment.

If you want to stay safe, you may also want to try:
Sunlight helps your body produce vitamin D, so blocking the sun from reaching your skin may mean that your body makes less of this nutrient. If you are careful about protecting yourself from the sun, you may want to consider getting vitamin D from a supplement or multivitamin, or eating foods such as dairy products that have been fortified with this vitamin.
A skin cancer screening is an exam in which you, a doctor, or a nurse checks the skin all over your body for signs of cancer, including moles or marks that have an unusual size or color. Screening may help you find skin cancer early, which could lead to a better outcome.
You may want to ask your doctor if they recommend that you undergo skin cancer screening. It may be a good idea for people with skin cancer risk factors.
You can also perform your own screening at home. Check all of your skin, including near your genitals, under your breasts, on your scalp, between your fingers and toes, and underneath your nails. You will need a mirror in order to properly check some areas. Talk to your doctor if you notice any new bumps, sores that don’t heal, or moles that are irregularly-shaped, painful, oozing, or bleeding.
If you spend a lot of time in the sun, or you have a history of sun exposure, it helps to know skin cancer symptoms so you know what to watch out for.
When looking for signs of skin cancer, think “ABCDE“:
Research clearly shows that regularly using sunscreen can reduce your chances of being diagnosed with skin cancer. It can also help prevent signs of premature aging. However, it is not the only thing that can help protect you from the sun’s UV rays — using other strategies like wearing protective clothing and staying in the shade can all play a role in keeping you safe and healthy. If you would like a skin-check, please make an appointment with Dr. Connor.


The digestive system breaks down and uses most parts of the food we eat. However, there are some substances that can’t be digested. Anything that can’t be broken down and is left over in the large intestine after a meal is digested is called “residue.”
Residue is mostly made up of fiber. Dietary fiber is a substance made by plants. It is primarily present in plant-based foods like grains and produce. The body can’t break down fiber.
Most people need to eat a lot of fiber in order to maintain good health. Eating more fiber reduces a person’s risk of chronic disorders like diabetes, heart disease, and cancer. The Academy of Nutrition and Dietetics recommends a daily fiber intake of 25 grams for women and 38 grams for men. However, a person may occasionally need to eat smaller amounts of fiber for health reasons.
The goal of a low-residue diet is to eat foods that can be easily broken down by the body and will lead to less residue left over in the digestive system. This diet typically causes people to have smaller, less frequent bowel movements.
A low-residue diet is very similar to a low-fiber diet, but they may not be exactly the same. Low-residue diets do focus on low-fiber foods, but they may also eliminate other types of foods as well. For example, dairy products do not contain much fiber, but still lead to a lot of residue, so these foods may also be avoided. This is important to note if you are following a low-residue diet for the purposes of bowel preparation, dietary or other health reasons.

Some people need to follow a low-residue diet before going through medical procedures. One such procedure is a colonoscopy. During this test, a physician uses a thin tube with a camera on the end to look inside the large intestine. Colonoscopies are used to diagnose certain illnesses and digestive problems. Colonoscopies are also an important part of screening for colon cancer. People with an average risk of developing this cancer should begin getting screened at the age of 45. Before a colonoscopy, a person needs to clean out their bowel. Traditionally, many physicians recommended a bowel prep that involved taking laxatives and consuming only clear liquids for one or more days before the procedure. However, in recent years many researchers have conducted clinical trials looking at other bowel prep methods. Several studies have found that people who ate a low-residue diet before undergoing procedures had equal or better colon cleansing compared to people who followed a clear liquid diet. Additionally, people following a low-residue diet preferred this method and were more likely to stick to the instructions. Physicians may also recommend following a low-residue diet before other intestinal tests. By eliminating leftover residue from the large intestine, this diet can help the physicians see the intestine more clearly and more accurately identify any problems.
Eating low-residue foods may help manage symptoms of conditions that affect the digestive system. Physicians may recommend following this eating plan to people who are dealing with:
There are two different disorders that fall under the umbrella of inflammatory bowel disease (IBD): ulcerative colitis and Crohn’s disease. In both of these conditions, there is ongoing inflammation in the small or large intestine. Over time, this inflammation causes damage and leads to symptoms like abdominal pain, diarrhea, constipation, blood in the stool, weight loss, and tiredness. However, these symptoms don’t occur all of the time. They occur or get worse during disease “flares.” Low-residue diets may help reduce the amount of stool, allowing the intestines rest and leading to fewer IBD symptoms during these flares. Diverticulitis is a condition in which small bulges or pouches form in the intestines, and then — these outpouchings — become inflamed. One study has found that eating foods that are easier on the digestive system, including low-fiber foods, may help reduce symptoms. Irritable bowel syndrome (IBS) is a disorder without a clear cause that leads to several digestive symptoms, including bloating, cramping, constipation, and diarrhea. In the past, most physicians have recommended that people with IBS try eating more fiber. Unfortunately, this can sometimes make symptoms more severe. Now, researchers are finding that a low-fiber diet can lessen symptoms or make them disappear altogether. A low-residue or low-fiber diet may also be necessary before surgery — either surgery on the intestines or gynecological surgery. Following a low-residue diet before these surgeries can help create more room in the abdomen and reduce risk of infection. Additionally, switching to a low-residue diet after intestinal surgery can help people’s intestines begin working again more quickly, leading to a shorter amount of time spent in the hospital.

During a low-residue diet, you’ll want to focus on low-fiber foods. This list of foods provides a good starting point for what you may be able to eat. However, each person digests food differently, so your physician may tell you to avoid foods that are on this list. Always follow your physician’s recommendations. Usually, the foods on this list have low levels of fiber. However, it is still important to check the nutrition facts label for everything that you eat. Some naturally low-fiber foods have extra fiber added in. When it comes to grains, white or refined products have less fiber than whole-wheat and whole-grain products. Stick to:
Most cooked, tenderized meats are okay to have on a low-residue diet. You can also have poultry and eggs. For plant-based options, you can try tofu and smooth peanut butter. Most fruits and vegetables should not be eaten raw. Cooking produce, removing skins and seeds, and avoiding pulp helps you cut back on fiber and residue. Vegetables that can be eaten raw include small amounts of zucchini, cucumbers, or lettuce. Make sure to peel and remove seeds first. You can also have cooked, canned, or juiced versions of the following vegetables:
When it comes to fruits, juices are always a good option — but make sure to buy pulp-free! Sauces and purees like applesauce are also good bets. Raw melon, cantaloupe, bananas, apricots, nectarines, peaches, and plums are usually okay to have on a low-residue diet. If you’re eating raw fruit, make sure it’s very ripe. You can also have canned fruits as long as they don’t come in heavy syrup. Make sure to drink plenty of fluids while on a low-residue diet. This can help prevent constipation, which is common when eating low-fiber foods.
Avoid whole-grain and whole-wheat foods, which contain a lot of fiber. Additionally, stay away from:
When it comes to meats, stay away from processed meats like hot dogs and sausage, and say no to any deli meats. You should also avoid nuts and crunchy peanut butter, beans, and tempeh, as these are all high-fiber foods. Avoid any vegetables that aren’t on the above lists. Additionally, stay away from any vegetables that haven’t been de-seeded or peeled. When it comes to fruit, you should avoid all dried fruits, as these typically contain a lot of fiber. You should also choose not to eat any pineapple, berries, figs, and prunes. Ask your physician whether it is okay to eat dairy products. Some low-residue diet recommendations include limiting or avoiding milk, yogurt, and cheese. These products contain low amounts of fiber but may worsen digestive symptoms and increase the amount of stool that you produce.

If you have only been eating low-fiber foods for a day or two, it may be fine to eat a normal amount of fiber again the next day. Ask your physician for recommendations.
If you have been following a low-residue diet for a longer time period, don’t go back to your usual diet immediately. It will be difficult for your digestive system to handle. Instead, increase the amount of fiber you eat gradually over time. Try eating a small amount of a high-fiber food for a couple of days in a row. If you don’t experience any symptoms, add this food back into your diet.
Some experts recommend adding 5 more grams of fiber to your diet each week. For example, if you have been eating 10 grams of fiber each day, try eating 15 grams of fiber per day the following week, and 20 grams per day the week after that. If you begin to experience digestive symptoms like bloating, cramping, or diarrhea, try decreasing your fiber intake again until the symptoms resolve.
A low-residue diet is similar to a low-fiber diet. In some cases, they may be the same. These diets may be a necessary tool when preparing for certain medical procedures. They can also be a helpful way of managing symptoms for people with digestive diseases. However, people should not usually stay on low-residue diets for long time periods, because fiber helps keep you healthy and prevent chronic illnesses. Follow your physician’s instructions when it comes to beginning and ending a low-residue diet, and heed their recommendations about what to eat and avoid. If you think this is a diet that could benefit you, please discuss with Dr. Connor first by making an appointment.
The prostate is a gland found inside the pelvis, underneath the bladder, and surrounding the urethra (the tube that carries urine from the bladder out of the body). The prostate makes part of the semen, the fluid that contains sperm. In young adults, the prostate is about the size of a walnut. However, it continually grows larger with age, potentially reaching the size of a lemon by the age of 60. In some cases, it may grow too large, leading to an enlarged prostate, also called benign prostatic hyperplasia (BPH). If the enlarged prostate presses against the bladder or urethra, it can lead to some health problems. BPH is not cancer, and men with an enlarged prostate don’t have a higher chance of being diagnosed with cancer. However, some of the symptoms of BPH overlap with those of prostate cancer, so it is important to be aware of any health changes and tell your doctor about any potential symptoms that you notice.

It is important to get early symptoms checked out to make sure they are not signs of cancer. Additionally, if urination problems go untreated, they can eventually lead to more serious issues such as bladder or kidney damage, urinary tract infections (UTIs), bladder stones, or kidney failure. Keep an eye out for symptoms of more serious conditions, such as an infection. Seek medical care right away if you have a fever, bloody urine, are urinating less than you usually do, or notice pain in your abdomen, side, or back. If you are experiencing any changes in your urination patterns, talk to your healthcare provider. They may try to figure out the cause of the problem by performing a physical exam or ordering various tests, such as:

There are also certain risk factors that can increase a person’s chances of developing an enlarged prostate. These include:
There are several possible BPH treatment plans that doctors may recommend. The approach that is right for you depends on several factors, such as how severe your symptoms are, whether your symptoms are disrupting your daily life, and your overall health.
Regardless of which treatment plan you choose, experts recommend that you visit your doctor at least once per year if you have an enlarged prostate. Regular check-ups provide the opportunity to switch up your treatment plan if needed.
If you don’t have BPH symptoms, or if your symptoms are mild, your doctor may recommend a “watchful waiting” or “watch and wait” approach. This means that you don’t use any treatments.
During this time, you should visit your doctor regularly so that they can keep an eye on your condition and make sure it isn’t getting worse or leading to other serious problems. If your symptoms start to get more severe, you may then decide that you want to try other treatments.

Some men turn to herbs, supplements, or natural products to ease BPH symptoms. If you choose to go this route, make sure to tell your doctor about everything that you are taking. Some natural products may interact with other medications or supplements or lead to side effects. Early studies found that saw palmetto may help ease symptoms of an enlarged prostate. This substance comes from the American dwarf palm tree, found in the southern parts of the U.S. However, when researchers tested saw palmetto in clinical trials, they found that there was no difference in BPH symptoms when men took saw palmetto compared to a placebo (sugar pill). In additional clinical trials, researchers tested increasingly high doses of saw palmetto, but still saw no effect. On the other hand, a more recent clinical trial found that men found symptom relief when they used saw palmetto oil that contained beta-sitosterol. Other research has also found that beta-sitosterol on its own may lessen urinary symptoms caused by an enlarged prostate. Older research also suggests that Pygeum africanum may help. Studies reported that men who used this supplement, which comes from the bark of the African plum tree, were more than twice as likely to say their symptoms got better compared to men who took a placebo.

Alpha blockers such as Cardura (doxazosin) and Flomax (tamsulosin) relax muscles in the pelvis near the prostate. This can help urine move through the urethra more easily. While these medications don’t affect the size of the prostate, they can often relieve symptoms quickly. Some men who take these medications may experience side effects such as headache, dizziness, or tiredness.
Proscar (finasteride) and Avodart (dutasteride) are 5 alpha-reductase inhibitors, medications that actually shrink the prostate. They do this by blocking an enzyme that helps make more DHT hormone. Because DHT triggers prostate cells to grow more quickly, lowering levels of this hormone leads to a smaller prostate and fewer symptoms. These medications may take a few months to relieve symptoms and may not be suitable for people with more severe BPH. Potential side effects of 5 alpha-reductase inhibitors include decreased libido and erectile dysfunction, although these problems are not common.
Phosphodiesterase-5 inhibitors such as Viagra (sildenafil) and Cialis (tadalafil) are erectile dysfunction medications that can also help treat BPH. These work by relaxing the muscles in the penis. This may help urine flow out more easily.
Some scientific studies have found that using multiple types of medication together may help lead to even better results. For example, doctors may recommend taking both an alpha blocker and a 5 alpha-reductase inhibitor. However, phosphodiesterase-5 inhibitors can interact with alpha blockers, so let your doctor know if you are using these medications.
In some cases, an enlarged prostate may occur along with prostatitis (inflammation of the prostate). This condition is sometimes caused by infection, so taking antibiotics can sometimes lead to symptom relief.
Doctors may recommend surgery for more severe cases of BPH that are causing problems like incontinence, bloody urine, frequent infections, or kidney problems. It may also be a good solution when medication isn’t working.
The most common surgery for an enlarged prostate is transurethral resection of the prostate (TURP). This procedure is generally safe and effective. It involves inserting a thin tube into the urethra and using it to remove excess prostate tissue.
In some cases, doctors may recommend other types of surgery. One possibility is transurethral incision of the prostate (TUIP), in which a surgeon makes a few small cuts in the prostate in order to help widen the urethra. In laser surgery, a tiny laser is passed through the urethra and used to get rid of prostate tissue. An open prostatectomy involves making a cut through the skin and removing all or part of the prostate gland.
Several kinds of minimally-invasive surgical procedures may also be an option. These procedures often involve using heat or electricity to destroy prostate tissue. Minimally-invasive surgeries may be a good
It’s important for each individual to work with their doctor to figure out the best treatment plan — what works best for you may not be a good fit for someone else.
For milder cases of an enlarged prostate, lifestyle changes, supplements, or certain medications may be enough to relieve symptoms. If these solutions aren’t enough, other medications or surgery may be more helpful. Additionally, it’s important to tell your doctor about any changes in urination. Even mild symptoms can occasionally be a sign of a more serious condition.
If you are having any of the symptoms above, or have other questions about your prostate, make an appointment with Dr. Connor.

Of course, there’s no way to permanently halt the aging process. However, eating right and taking care of yourself can help minimize age-related damage and keep you feeling as good as you can throughout many decades of life.
(I encourage you to read my entire series on superfoods to learn about what is so super about superfoods as well as about superfoods for weight loss, heart health, diabetes and pre-diabetes, radiant skin and gut health.)
Every part of your body goes through age-related changes. Your skin loses its elasticity, your muscles become weaker, and your bones lose strength.
Additionally, the older you get, the higher your risk for health conditions such as:
Adopting healthy habits, including eating more nutritious foods, may help slow down these changes and keep you as healthy as possible as you age.
Experts are still learning about the many factors that bring about aging. However, they have identified a few possible causes, which may be affected by lifestyle habits such as diet.
Some genes help control aging. These genes may be turned on or off or develop mutations that lead to age-related changes within cells.
Aging is also linked to damage. Small molecules called reactive oxygen species (ROS) can form within cells. ROS damage DNA and cells, causing a cell to age. On the other hand, antioxidants are substances that get rid of ROS, helping prevent and heal damage. Some unhealthy foods can lead to higher levels of ROS, while other foods can act as antioxidants, keeping your cells young.
Inflammation is another factor that leads to aging. A little bit of inflammation is necessary to help the immune system fight off germs or toxins. But chronic (ongoing) inflammation can accelerate the aging process and lead to age-related health problems. Different foods can help raise or lower the amount of inflammation in the body.

There’s no one definition of a “superfood,” but the label tends to be given to foods or drinks that offer higher levels of health-boosting nutrients. Superfoods also frequently contain helpful molecules like antioxidants, which protect cells from free radicals and help heal the damage that builds up with age. Additionally, many superfoods have been shown to help reduce the risk of developing different chronic diseases.
Adding more of these foods to your diet may help you keep your body healthy and make you look and feel as young as possible as you age!
Blueberries are a powerful superfood that can help keep you healthy into your later years. These fruits contain antioxidants and other anti-aging molecules.
Blueberries can protect nerve cells from ROS and inflammation. This can help prevent or even reverse age-related problems with memory, cognitive abilities, balance, and motor function.
Blueberries also contain molecules called anthocyanins that help protect against disorders like diabetes and heart disease. They may even help protect against early death.
Different kinds of nuts — including almonds, walnuts, pistachios, Brazil nuts, and pine nuts — provide healthy fats and protein and help protect against inflammation. Another big benefit of eating nuts is their ability to help prevent age-related health conditions such as diabetes, heart disease, and cognitive problems like Alzheimer’s disease and dementia.
Nuts may even help you live longer. One study found:
Pomegranates are a fantastic superfood that contain several anti-aging molecules.
Several substances found in pomegranates can help protect cartilage from being degraded. This may help keep joints healthy and protect against arthritis.
These fruits also contain molecules called ellagitannin and ellagic acid. When you eat pomegranate, the good bacteria in your gut transform these chemicals into urolithin A (UA). UA reduces inflammation and gives a boost to the mitochondria (small structures that make energy for your cells).
UA can also protect against age-related problems that appear in your muscles, joints, brain, and other tissues. In some laboratory studies, UA also helped animals live longer, although this has not yet been tested in humans.
Eating more tomatoes may be an easy way to keep your skin healthy as you age. Tomatoes contain lycopene, a red pigment that also acts as an antioxidant. Pro tip: your body can absorb lycopene from tomato paste more easily than it can from fresh tomatoes.
Researchers have found that lycopene is present in your skin cells and in the oil that your skin produces, although levels decrease with age. Fortunately, eating more lycopene can increase how much of this molecule is present in your skin, bringing lycopene levels up to those seen in young adults. Studies have also found that eating more tomato paste protects the skin from sun damage.
Tomatoes may provide other benefits as well. Some research shows that eating more tomatoes can help reduce your chances of being diagnosed with serious conditions like heart disease and cancer.
Salmon, as well as other fatty fish like trout, mackerel, sardines, and tuna, is a great source of vitamin D, protein, and healthy fats, making it an important superfood.
Levels of vitamin D in the body tend to drop with age. This is bad news for your bones, since vitamin D is needed to keep them strong and healthy. Low vitamin D levels mean an increased risk of weak or broken bones. Not getting enough of this vitamin also puts you at risk for certain age-linked diseases like high blood pressure, diabetes, depression, and cancer. Making sure you have enough of this vitamin as you age is essential.
Healthy protein sources also become increasingly important as you age. The older you get, the more muscle mass you lose. Eating higher levels of protein can help combat this and keep the muscles healthy.
The omega-3 fats found in salmon and other fish also help with healthy aging. They can reduce inflammation and protect brain health, helping prevent age-related declines in thinking and memory abilities.
Milk and dairy products such as cheese and yogurt provide several important nutrients. Like fatty fish, milk is a good source of protein. In the United States, milk is also usually fortified with extra vitamin D, making it another good source of this vitamin.
Dairy foods also contain a lot of calcium, a mineral that is important for bone health. Low calcium levels can eventually lead to osteoporosis, a disease in which the bones become weak. Older adults may also be at risk for this condition because some medications may prevent the body from absorbing as much calcium as it normally would. Getting enough calcium from your diet is important at every age and can help prevent future bone problems.
People who want to age well should look to whole grains. Try switching out white bread for whole wheat bread, refined pasta for wheat pasta, and white rice for brown rice. You can also eat more grains like quinoa, oats, or popcorn.
Research shows that middle-aged adults who eat more whole grains are more likely to have better physical and mental health, and are less likely to have chronic illnesses.
Turmeric is the super spice that gives Indian curries their yellow color. Turmeric contains a molecule called curcumin that can help improve many aspects of health and has some anti-aging properties.
Laboratory studies have found that curcumin can help worms, flies, and mice live longer. It’s not yet clear whether turmeric can affect lifespan in humans, but researchers have identified several ways in which this spice can affect aging.
Curcumin can boost the body’s own natural antioxidants. It can also turn off several genes linked to aging. Finally, it can lessen symptoms of certain health conditions linked to aging and inflammation, such as heart disease, diabetes, and cancer.
While it may not be a “superfood” in the usual sense, water is an important nutrient that is vital for aging well. Your skin loses moisture as you get older, which makes it age. Staying hydrated is important for keeping all of your tissues healthy.
Your sense of thirst may also decrease as you get older, making it harder to remember to drink enough fluids. Additionally, staying hydrated is important when taking certain medications for chronic health conditions.
Make a plan to drink a certain number of glasses of water each day. Plan when you’re going to have drinks — don’t wait until you feel thirsty. Try having a full glass of water with every meal, and while taking any medication. If drinking enough water is difficult, you can also drink some low-fat or nonfat milk, or juice without added sugar or salt.

While eating superfoods can help protect against illness, following a healthy eating plan may provide even better results. Researchers have developed certain diets that reduce a person’s chances of developing conditions that may come on with age.
One of the best-studied diets is the Mediterranean diet. It emphasizes plant-based meals with lots of vegetables, fruits, whole grains, olive oil, and seafood. This diet can lower the risk of developing heart disease, diabetes, Alzheimer’s disease, and certain types of cancer. In one study, people who followed the Mediterranean diet more closely were 26% less likely to have an early death from heart problems.
A related diet, called Dietary Approaches to Stop Hypertension (DASH), helps lower blood pressure and cholesterol levels and boost heart health.
The Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet combines elements from both eating plans above. The MIND diet encourages people to eat leafy green vegetables, berries, whole grains, nuts, beans, and wine. It can help protect against Alzheimer’s disease and dementia.
Many different lifestyle factors affect how we age. If you want to maintain health into your later years, you may also want to consider making other changes.
Nearly one in three adults over the age of 50 are physically inactive. Additionally, people with chronic health conditions are more likely to report that they don’t get as much exercise. However, physical activity is very important — it can help prevent or treat many different disorders and reduce a person’s chances of an early death.
Experts make the following physical activity recommendations for older adults:
If you can’t reach all of the above goals, remember that doing something is better than nothing. The more time you spend moving and the less time you spend sitting, the better! Make sure to talk to your doctor before starting a new exercise plan to make sure that you are being active in a way that is healthy for you.
Smoking cigarettes and drinking alcohol can speed up the aging process. They can both negatively impact the skin and lead to more wrinkles. Alcohol and tobacco can also increase a person’s chances of being diagnosed with cancer and other serious conditions.
One study also found that people who didn’t drink heavily or smoke, and adopted other healthy habits like eating healthy and getting exercise, were 60% less likely to develop Alzheimer’s disease.
People of all ages can struggle with maintaining good mental health. However, problems like depression or anxiety can have a bigger impact on physical health for older adults. Poor mental health can make it harder for people to seek treatment for other conditions like diabetes or heart disease.
If you notice changes in your mood or emotions, talk to your doctor. Therapy or medication often helps improve your mental health, which can in turn have a positive impact on your physical health.
Your diet increasingly impacts your health as you age. The more you add superfoods and other nutritious foods to your diet, the more you can protect your skin and other organs from age-related damage and decrease your risk of chronic health disorders. Please click here to schedule an appointment with Dr Connor or call us at (512) 382-9500.

In an article in Giddy, Dr. Connor explains that although its primary function is reproductive system development and maintenance, estrogen also plays a key role in bone, breast and brain health, Connor said. Estrogen bolsters bone strength, and the lack of it can contribute to weak, brittle bones and osteoporosis. Read the entire article in Giddy. If you are concerned with bone strength and want to discuss it further, make an appointment with Dr. Connor.



Diabetes — a condition that affects more than one in 10 Americans — often leads to additional health problems called complications. One of the most common diabetes complications is peripheral neuropathy. People with this condition have nerve damage that leads to pain, tingling, numbness, or weakness in the hands and feet. About one in two people with diabetes have peripheral neuropathy.
Neuropathy is a disease of the nerves. The body uses nerves to communicate with the rest of the body. Some nerves send signals from the brain to other tissues, and then other nerves send signals back to the brain. This process helps the brain learn about feelings and sensations, tell muscles when and how to move, and control different processes in the body such as breathing and the heartbeat.
In people with diabetes, the body has a hard time controlling levels of sugar and fat in the blood. High blood sugar levels and high fat levels can directly damage the nerves and also harm the blood vessels that keep the nerves healthy. In people with neuropathy, the brain has a harder time receiving information from and sending signals to certain parts of the body.
Neuropathy can also be caused by other conditions. Certain genetic disorders that are passed down within families can lead to nerve damage. Other disorders such as Guillain-Barre syndrome, inflammatory conditions, or cancer may also lead to neuropathy. Environmental or lifestyle-related causes of neuropathy can include heavy drinking, not getting enough of certain vitamins or minerals, exposure to toxic substances, or infections.
Damage to different types of nerves can lead to different forms of neuropathy. These include:
People with diabetes can develop any of these neuropathies. Peripheral neuropathy is the most common type of nerve damage.

These symptoms can develop and worsen slowly over time, or they can appear quickly. They may be more severe at night than they are during the day.
Over time, people with diabetic peripheral neuropathy may experience worsening problems with their feet. When it is harder for the nerves in the feet to pick up on different sensations, a person may be less likely to notice pain or discomfort. Some people with diabetes develop sores, blisters, or infections on their feet, and may not notice these issues right away.
Diabetes interferes with the body’s healing processes by preventing enough blood from flowing to injured tissues. This means that it is harder for the body to repair even minor injuries. Some people with diabetes who develop severe foot problems may need to have a toe or foot amputated.
When feet and leg problems pile up, it may become harder to walk. Some of those with neuropathy may have a hard time balancing properly. This can lead to falls, which puts a person at risk for breaking bones. A person’s sense of movement may also be affected. Peripheral neuropathy may also cause a lot of pain, especially while walking.
Diabetics with peripheral neuropathy are likely to need more frequent visits to their doctor’s office or the hospital. They may also have a hard time working because of pain or difficulties getting around. All of these issues can in turn lead to mental health disorders such as anxiety or depression.

Blood tests are often a part of physical exams. These tests can identify various health problems that can cause neuropathy or be found in people with diabetes. Blood tests may be used to detect:
During the physical exam, your doctor may perform several tests to see whether you are able to detect sensations with the nerves in your feet. One possible test is a monofilament test, in which the doctor touches your feet with a thin strand of nylon to see if you can feel it. Another test involves touching the feet with a tuning fork to see if the nerves in your feet can sense vibrations.
Doctors can directly measure how well your nerves and muscles are working with other tests. They may use nerve conduction velocity tests (NCV) to see how fast your nerves are able to send out signals. An electromyogram (EMG) measures electricity in the muscles, which helps doctors understand how fast your muscles respond to signals from the nerves.
Other tests may include checking your balance, seeing how well you walk, or testing the blood flow in your feet and toes.

One of the most important ways people can reduce their risk of neuropathy is by treating their diabetes. Keeping blood sugar levels under control helps prevent the nerves from becoming damaged. Work with your doctor to develop a diabetes treatment plan that works for you.
Certain risk factors can increase a person’s chances of developing diabetic peripheral neuropathy. These include:
You can’t control some peripheral neuropathy risk factors like age or genetics. However, you can reduce your risk of nerve damage by focusing on certain lifestyle changes. Getting more exercise, eating a balanced diet (especially superfoods for diabetics), quitting smoking, and limiting how much you drink may help you avoid peripheral neuropathy. Additionally, use lifestyle changes or medication to prevent or treat high blood pressure or cholesterol levels.
If you are suffering from neuropathy pain, the first step is talking to your doctor, who can help you come up with a treatment plan. Make sure to ask about ways to both treat the neuropathy as well as keep your diabetes under control to prevent further damage.
Several different types of drugs can help manage peripheral neuropathy pain. However, traditional painkillers may not always be the best option. In particular, over-the-counter pain medications often do not work for neuropathic pain. These include non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen as well as other drugs like acetaminophen.
Instead of utilizing traditional pain relievers, physicians sometimes recommend a medication for nerve pain that is in the “antidepressant” category of medicine because of the mechanism of action of this medication. These medications don’t heal nerve damage, but they can reduce neuropathy symptoms. Possible options may include:
Anti-seizure medications may be another option for treating peripheral neuropathy pain. These drugs may include Neurontin (gabapentin) or Lyrica (pregabalin). Finally, topical medications that are applied directly to the skin may help. Your doctor may be able to prescribe a cream, spray, or patch that can numb pain.
These medications are not always equally effective for everyone. If you try one medication and it doesn’t seem to be helping, notify your doctor — another drug may work better for you.
When blood sugar levels rise, some of these medications may not work as well to treat neuropathy symptoms. Following your diabetes treatment plan is important when trying to treat nerve pain and treating the root cause of the problem is the goal in working to reduce neuropathy and neuropathic pain.
Several studies have found that alpha-lipoic acid can work well to treat neuropathy symptoms. This molecule is an antioxidant that is made by the body. Alpha-lipoic acid treatments are especially effective when they are given intravenously, through an IV needle that goes directly into a vein.
This antioxidant is also available as an over-the-counter supplement. In this form, alpha-lipoic acid may still help with symptoms, but it is not usually as effective as IV treatments.
People with diabetic neuropathy may want to consider going to physical therapy (PT). This type of treatment can help you build strength and improve your balance. During PT, you will work with a physical therapist to perform different exercises that specifically address your needs.

Taking good care of your feet can help prevent minor problems from getting worse. Doctors recommend that people with peripheral neuropathy check their feet every day. If you notice a small issue right away and seek treatment, you have a better chance of healing and avoiding infection. Try looking for:
Try to get into the habit of washing your feet each day. Make sure the water that you use isn’t too hot. If you have a hard time sensing temperature, use a thermometer to measure the water before washing. Don’t use water above 95 degrees Fahrenheit (35 degrees Celsius). Once you are done, dry your feet thoroughly. Dust your feet with baby powder or cornstarch to help keep your skin dry.
Another way to protect your feet is always wearing socks and shoes. Socks can help keep your feet dry, while shoes protect your feet from injury. Make sure your shoes aren’t too tight, and break in new shoes by wearing them for short periods of time when you first get them. Before putting on your shoes, check that there are no small stones or other objects inside that could hurt your feet.
Certain types of footwear can also help prevent ulcers. Ask your doctor about whether insoles, shoes, or orthotics may help support your feet.
A yearly foot exam is also a good idea for people with peripheral neuropathy. During this visit, your doctor can make sure your feet are in good health. More frequent exams may be needed for people who have current or past foot problems. You may be able to go to your primary care provider for this exam, or your doctor may recommend that you see a podiatrist (a doctor who specializes in treating feet).
Managing your blood sugar levels is a very important part of treating and controlling nerve damage. Make sure to check your blood sugar regularly. Choose nutritious foods that won’t lead to large blood sugar spikes, and get regular physical activity. Additionally, use any medications as directed by your doctor.
If you don’t think that you are controlling your blood sugar levels well enough, talk to your health care team. Your doctor may be able to help you better understand which treatments or lifestyle changes will help prevent complications from diabetes. A certified nutritionist or registered dietician can also help you come up with a better eating plan.
It is important to take peripheral neuropathy seriously, since symptoms can get worse and may cause additional problems over time. Effectively treating your diabetes can help you avoid nerve damage or prevent existing symptoms from worsening. Medications can help relieve symptoms of peripheral neuropathy, including pain. Follow the directions of your health care team when it comes to making necessary lifestyle changes and taking care of your feet. If you are having nerve pain and would like to discuss it further, please make an appointment.