Are you avoiding the Doctor Due to the Pandemic?
The Serious Implications and How You Can Safely Get Medical Care
Many people are trying to be responsible during the COVID-19 pandemic by limiting their interactions with other people and by not going out in public spaces as often. However, one result of these precautions is that some people have been avoiding going to their physician or getting medical care. This can lead to serious consequences for those who are experiencing other health problems. Thankfully, there are several alternatives to in-person healthcare visits when appropriate, and there are also several ways to reduce your risk of infection for those times when you need to go to the hospital or your doctor’s office.
Have People Been Avoiding the Doctor?
Many people report that someone in their household has put off medical care due to the pandemic. People are starting to feel more comfortable going to their doctor’s office but are still seeking less health care than they did a year ago, according to many surveys nationwide.
Why is this?
It’s possible that people may need slightly less medical attention than they did in past years. With more people working from home and fewer people going out socially during COVID-19, the number of traffic accidents has decreased across the nation, thankfully. Some people may be eating out less and perhaps (hopefully?) cooking healthier meals at home as well so might need less medical care related to that these days. Also, in this year with the COVID-19 pandemic, surgeons had to cancel procedures, physicians had to temporarily close medical offices, and many also had to adjust their schedule in order to see fewer patients for proper cleaning to take place. Some patients may have wanted to see a doctor but couldn’t visit their usual providers for many different reasons.
Additionally, many people lost their jobs, were laid off, or took pay cuts during the pandemic. These factors have caused some Americans to lose their health insurance or to have a hard time continuing to pay for medical care. Many patients have put off getting tests or receiving treatment for chronic illness. However, research has shown that people are also actively avoiding getting medical attention when they need it – and sometimes when they need it most. By now, we all know that social distancing and isolating from other people are important public health measures that can reduce the spread of the coronavirus. Many people may be especially worried about coming into contact with other potentially contagious people in a doctor’s office or hospital. But … wait, there can be serious health consequences of avoiding going to your doctor!
When people avoid getting medical care, there may be long-term consequences. According to a recent article in JAMA (Journal of The American Medical Association, a peer reviewed medical journal), between March and July of this year, nearly 250,000 more people died than expected in the United States. According to this article, two-thirds of these deaths were due to COVID-19, but the other one-third was due to causes like heart attack. This means that many more people were dying from other health conditions than “normal” years’ numbers would indicate.
Many people who experienced symptoms of serious health problems did not seek emergency care due to fear of getting infected with the coronavirus. Within the first ten weeks of the pandemic, emergency department visits decreased for heart attack, stroke, and diabetes. Clearly, not receiving help during a medical emergency can be dangerous. People who have a heart attack are more likely to survive and have less heart damage if they get medical attention ASAP… and this is true for someone who is having a stroke as well. Strokes can cause brain damage, and the faster a person gets help, the better he or she will do in recovery. While most people might realize this, a prevailing feeling of fear toward the coronavirus has reduced the number of patients who seek care when they need it most.
Getting regular checkups is also important for preventing more serious disease. Screenings for cancer have decreased this year for many reasons already mentioned.
Many of us in health care are concerned about these trends. Even the American Heart Association created their “Don’t Die of Doubt” Campaign to encourage people to continue to get medical care when needed—and especially for more urgent health concerns.
So … what do you do?
Weigh Your Risk
The risks and benefits of getting medical care should be thoughtfully considered.
Certain people are at high risk for having severe symptoms if they contract COVID-19 or even the flu. These folks need to take extra precautions to avoid coming into contact with sick people. We know this, of course, but these people need medical care too! Obtaining proper medical treatment can reduce the risk to these people of serious health complications
Certain types of check-ups or treatments can more easily be delayed than others. There are also ways people can still receive medical treatment while reducing their risk.
Work with your physician to decide which options are best for your health.
Alternatives to In-Person Medical Care
Delaying Treatment
Some routine or preventative healthcare visits may be able to be delayed, but check-ups may not be able to be delayed- and specific medical screenings need to happen … so please talk to your physician about the risks and benefits of delaying healthcare visits based on your particular needs. In-person visits are also very important for certain age groups—such as for newborns, infants, and toddlers. Keeping up to date on vaccines is essential, so have the conversation with your physician.
Telemedicine
Thankfully, you don’t always need to see someone in-person to receive healthcare. People who continue to need medical care during this time can take advantage of telemedicine options, (again – when appropriate) as this works great for many medical conditions. Telemedicine makes use of phone calls, online video calls, smartphone apps, or text messages. Virtual visits can be used for a wide variety of health services, such as:
- Acute urgent care for conditions that are not life-threatening
- Monitoring chronic health conditions
- Mental health services
- Health coaching and counseling
- Physical or occupational therapy
- Follow-up appointments after hospitalization, surgery, or changes in medication
Technology in this area has been rapidly improving, making it easier for providers and patients to connect and increasing numbers of health insurance companies are expanding their coverage for “virtual” or remote care. Prescriptions can often be handled entirely over the phone. Physicians may be able to prescribe new medicines virtually and also follow up with patients in this manner to see how new drugs or dosages are working out. There are even online pharmacies that can help you avoid having to pick up medications in person…and many of our local awesome Austin pharmacies are offering delivery services as well!
How to Access In-Person Care Safely During the COVID-19 Pandemic
How Risky is In-Person Care?
In general, your risk of getting COVID-19 increases when the people around you aren’t following basic precautions. Medical clinics and hospitals have adopted new precautions to help keep patients safe. For example, many healthcare offices screen patients before they enter the building by taking their temperature or by asking them questions about whether they have recently experienced COVID-19 symptoms or had sick contacts. Many doctor’s office and clinics have a separate waiting room for people who are visiting due to possible viral infections or may see possible COVID cases at specific times throughout the day. In my practice, I test people who might be sick from the coronavirus or the flu from the ‘comfort’ of their vehicle, and many other physicians are doing the same. Your risk of getting COVID-19 from a healthcare setting is likely much less than it is in most other public spaces. Also, in my practice, I often see people by telemedicine to triage what testing or evaluation might be needed before they come to my office. This lessens risk to them, to me and my staff, and to others who might be using our building.
Prepare Ahead of Time
In a non-emergency situation, you can take precautions ahead of time to help ensure your doctor’s visit is safe and goes smoothly. You may want to read up on any possible new policies that your physician has recently put into effect. For example, some doctor’s offices may have previously allowed other people to accompany you during visits, but now limit the number of other visitors. If you’re concerned about being exposed to COVID-19, ask your physician’s office a few questions before you arrive for your appointment, such as:
- Is there any paperwork that needs to be filled out that I can complete ahead of time?
- Can I check in via phone or text and wait in my car rather than in the waiting room?
- What are the requirements regarding mask wearing and social distancing during my appointment?
- How often do you clean exam rooms and common areas?
- Are other people, such as caregivers or children, allowed during my visit?
- Does this visit need to be in person, or can it be handled virtually through telemedicine?
Staying Safe During Your Visit
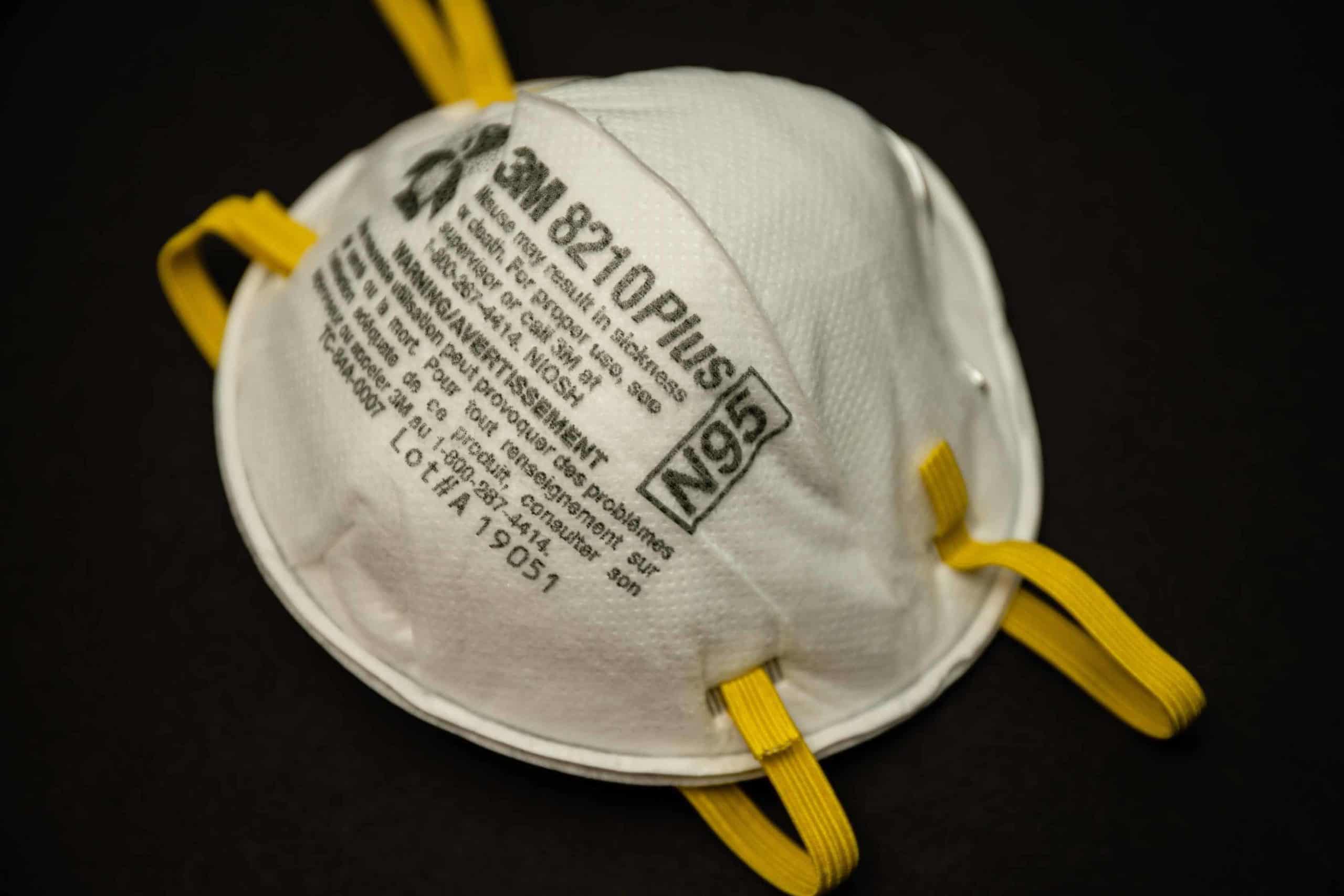
#Mask up! Put on your mask before you enter the building where your medical visit is going to occur. Make sure your mask covers both your mouth and your nose. If you don’t have a mask, ask whether your healthcare provider can give you one.
Social distancing is usually possible in doctor’s offices, and many facilities have signs or stickers on the floor to help you visualize how far apart to stand when checking in. Additionally, while in waiting rooms, you can sit a few chairs away from others.
You can also stay safe by reducing how often you touch any surfaces. For example, you may be able to hit elevator buttons with your elbow. When checking out after your appointment, ask if touchless or online payments are an option. Additionally, avoid touching your face or mask while you’re in the building. Once your visit is over, wash your hands before taking your mask off.
Getting Help In An Emergency
In case of a serious health issue, please don’t delay getting care. Every minute can count when it comes to problems such as heart attack, stroke, or a diabetic emergency. These conditions have a higher chance of leading to serious complications or death compared to COVID-19, so the hospital should not be avoided if you need the care. If you’re not sure whether your situation constitutes an emergency, try to call your physician, a nurse hotline, or 911, and ask for additional advice. And, remember, getting urgent medical care is still urgent.
*Brynna Connor, MD is a board-certified physician who practices in the Austin, Texas area with creative, family-oriented medicine. She has special interest in wellness, preventative medicine, and anti-aging and regenerative medicine. Dr. Connor may be reached at 512.382.9500, or schedule a consultation online.
Follow me on Twitter at @doctorbconnor